How do vaccines work?
Meta assessment by Chukwuma Chinaza Adaobi
This article is part of a series of explainers on vaccine development and distribution. Learn more about vaccines – from how they work and how they’re made to ensuring safety and equitable access – in WHO’s Vaccines Explained series.
Germs are all around us, both in our environment and in our bodies. When a person is susceptible and they encounter a harmful organism, it can lead to disease and death.
The body has many ways of defending itself against pathogens (disease-causing organisms). Skin, mucus, and cilia (microscopic hairs that move debris away from the lungs) all work as physical barriers to prevent pathogens from entering the body in the first place.
When a pathogen does infect the body, our body’s defences, called the immune system, are triggered and the pathogen is attacked and destroyed or overcome.
The body's natural response
A pathogen is a bacterium, virus, parasite or fungus that can cause disease within the body. Each pathogen is made up of several subparts, usually unique to that specific pathogen and the disease it causes. The subpart of a pathogen that causes the formation of antibodies is called an antigen. The antibodies produced in response to the pathogen’s antigen are an important part of the immune system. You can consider antibodies as the soldiers in your body’s defence system. Each antibody, or soldier, in our system, is trained to recognize one specific antigen. We have thousands of different antibodies in our bodies. When the human body is exposed to an antigen for the first time, it takes time for the immune system to respond and produce antibodies specific to that antigen.
In the meantime, the person is susceptible to becoming ill.
Once the antigen-specific antibodies are produced, they work with the rest of the immune system to destroy the pathogen and stop the disease. Antibodies to one pathogen generally don’t protect against another pathogen except when two pathogens are very similar to each other, like cousins. Once the body produces antibodies in its primary response to an antigen, it also creates antibody-producing memory cells, which remain alive even after the pathogen is defeated by the antibodies. If the body is exposed to the same pathogen more than once, the antibody response is much faster and more effective than the first time around because the memory cells are at the ready to pump out antibodies against that antigen.
This means that if the person is exposed to the dangerous pathogen in the future, their immune system will be able to respond immediately, protecting against disease.

How vaccines help
Vaccines contain weakened or inactive parts of a particular organism (antigen) that trigger an immune response within the body. Newer vaccines contain the blueprint for producing antigens rather than the antigen itself. Regardless of whether the vaccine is made up of the antigen itself or the blueprint so that the body will produce the antigen, this weakened version will not cause the disease in the person receiving the vaccine, but it will prompt their immune system to respond much as it would have on its first reaction to the actual pathogen.

Some vaccines require multiple doses, given weeks or months apart. This is sometimes needed to allow for the production of long-lived antibodies and the development of memory cells. In this way, the body is trained to fight the specific disease-causing organism, building up the memory of the pathogen so as to rapidly fight it if and when exposed in the future.
Herd immunity
When someone is vaccinated, they are very likely to be protected against the targeted disease. But not everyone can be vaccinated. People with underlying health conditions that weaken their immune systems (such as cancer or HIV) or who have severe allergies to some vaccine components may not be able to get vaccinated with certain vaccines. These people can still be protected if they live in and amongst others who are vaccinated. When a lot of people in a community are vaccinated the pathogen has a hard time circulating because most of the people it encounters are immune. So the more that others are vaccinated, the less likely people who are unable to be protected by vaccines are at risk of even being exposed to harmful pathogens. This is called herd immunity.
This is especially important for those people who not only can’t be vaccinated but may be more susceptible to the diseases we vaccinate against. No single vaccine provides 100% protection, and herd immunity does not provide full protection to those who cannot safely be vaccinated. But with herd immunity, these people will have substantial protection, thanks to those around them being vaccinated.
Vaccinating not only protects yourself but also protects those in the community who are unable to be vaccinated. If you are able to, get vaccinated.


Throughout history, humans have successfully developed vaccines for a number of life-threatening diseases, including meningitis, tetanus, measles and wild poliovirus.
In the early 1900s, polio was a worldwide disease, paralysing hundreds of thousands of people every year. By 1950, two effective vaccines against the disease had been developed. But vaccination in some parts of the world was still not common enough to stop the spread of polio, particularly in Africa. In the 1980s, a united worldwide effort to eradicate polio from the planet began. Over many years and several decades, polio vaccination, using routine immunization visits and mass vaccination campaigns, has taken place in all continents. Millions of people, mostly children, have been vaccinated and in August 2020, the African continent was certified wild poliovirus free, joining all other parts of the world except Pakistan and Afghanistan, where polio has not yet been eradicated.
CLICK HERE TO JOIN MEDICINE PORTALS WHATSAPP GROUP FOR MORE NEWS UPDATES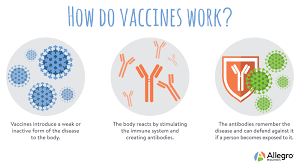



No comments:
Post a Comment